South Australian Medical Heritage Society Inc
Website for the Virtual Museum
Home
Coming meetings
Past meetings
About the Society
Main Galleries
Medicine
Surgery
Anaesthesia
X-rays
Hospitals,other organisations
Individuals of note
Small Galleries
Ethnic medicine
- Aboriginal
- Chinese
- Mediterran
Leucotomy and Psychosurgery
The Rise and Fall of a Promising Surgical Procedure.
Acknowledgements: We are most grateful to Professor Donald Simpson who was involved in the procedure and provided us with books, references slides and general information. David Buob kindly told us about the role that the Parkside Hospital (now Glenside) played in the surgery and the results of psychology reviews on patients who had leucotomy. Greg Sampson gathered the important references in the appendix.
The appendix gives the visitor access to additional information about the articles and names mentioned in the presentation. The history of Psycho-surgery is reviewed in chronological steps and paragraphs. Each mentions the time and the name of the contributor and a reference to the source.
We welcome any positive or negative comments.
Tony Slavotinek (article), Greg Sampson (appendix).
Introduction
The definitions of the words Psychosurgery and Leucotomy (Lobotomy in USA) first appeared in the supplement of the OED in 1987. Psychosurgery was defined as "Psycho + Surgery. Brain surgery intended to alter the behaviour of patients with certain kinds of severe mental stress or disorder".
Attempts to alter or modify human behaviour by physical means were initially tried by exposing the brain by removing a small section of the skull by trephining as early as 6,500 BCE. It is quite likely that this was done initially by using flints. Excavations found skulls with new bone formation confirming survival. The most likely indications were trauma, intolerable headaches and behavioural problems.
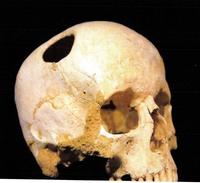
The smooth edges of the trephine suggest healing and survival.
Scientific approach to study of brain function was facilitated by emerging medical technologies, such as microscopy and tissue staining advances. Understanding of nerve conduction and anaesthesia followed. Additional helpful information became available from the studies of brain function after head wounds sustained at work or in conflicts such as WW1.
Jean Pierre Flourens (1794-1867), made localised lesions in the brains of rabbits and pigeons, and recorded their effects on their behaviour and motor and sensory function.
Pierre Paul Broca found that patients with speech defects had some damage in the lateral anterior frontal cortex which now bears his name, "Broca's area".
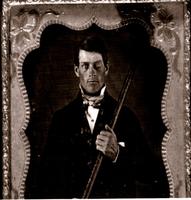
A case which records personality change after a massive brain injury is the report about Phineas Gage (1823-1860). As a foreman of a railway construction team in 1848, Gage used a crow bar to split a large rock. Apparently a spark caused an explosion. The crowbar entered his left cheek and perforated his frontal bone. Gage survived. His physical state appeared unchanged but his personality changed. He was more irritable, unstable and used foul language. Gage survived for 12 years, working as a coachman. Doctors J. M. Harlow and D. Ferrier reported on his injury and recovery.
There were other reports of personality change after lesions in the frontal lobes in patients and animals. The most encouraging was decrease in violent behaviour and decrease in pain and depression. There was an impressive demonstration in 1935 at the Second International Congress of Neurology when Jacobsen and Fulton from Yale presented two chimpanzees, Becky and Lucy, who had lesions in their frontal lobes, causing the loss of aggression and preventing tantrums.
The reports of behaviour changes in monkeys prompted Egas Moniz, a Portuguese neurologist, to suggest in 1936 that a lesion in the frontal lobes of the most severely affected mental patients should be tried. The date was 12-12-1935 and Pedro Almeida Lima was the surgeon. The result was gratifying.
People responsible for the development of leucotomy as a surgical procedure.
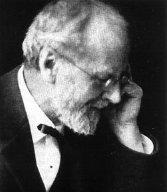
Egas Moniz studied medicine at the University of Coimbra. He specialised in neurology in Bordeaux and Paris. His first appointment as Professor of Neurology was in 1902, but within a year he entered politics and was in the Portuguese Parliament until 1913. He continued to teach as a neurologist and became a Professor of Neurology in Lisbon in 1911. He left politics in 1920. His first contribution was the use of intra-arterial Thorotrast to image the brain. His next advance was the publication of the results of 40 leucotomies on his patients. He claimed that: "Prefrontal leucotomy is a simple operation, always safe, which may prove to be effective surgical treatment in certain cases of mental disorder". He had supporters in the USA, and the procedure enjoyed a world wide vogue for a decade or more.
In 1949 he was awarded the Nobel Prize in Medicine and Physiology.
Lima was the surgeon who performed the leucotomies. His other interest was brain imaging with Thorotrast, and he published his results widely.
Other European countries adapted the procedure but were more cautious, and only a few procedures were performed in England before 1940. The Italians were more enthusiastic. Moniz came to Italy to demonstrate the procedure and the Italian press mentioned the procedure in 1936. About 200 leucotomies were performed by 1939 in the Racconigi Hospital near Turin. A new modification of the procedure using a trans-orbital approach was developed by Amarro Fiamberti using an approach to the frontal lobe through the eye socket and injecting alcohol or formalin. A leucotome was used later. This approach was later used by Freeman.
THE UNITED STATES EXPERIENCE
Walter Freeman, a neuro-psychiatrist from the George Washington University Hospital, and his surgeon J. W. Watts performed the first American leucotomy in November, 1936.
Freeman met Moniz in London in 1935 where they both attended the Second International Congress of Neurology. Moniz and Freeman corresponded, and Freeman used the information to develop the "Freeman-Watts" technique. Freeman was an over-enthusiastic proponent of the procedure and this influenced some of his reports. He believed that leucotomy was safe and produced an infantile behaviour in his patients.
Blackwell (Oxford) in 1942 published a book by Freeman and Watts entitled "PSYCHOSURGERY In the Treatment of Mental Disorders and Intractable Pain". Many patients were referred for the procedure, often from areas where there were no surgical facilities, and Freeman adopted an Italian procedure suggested by Fiamberti. In 1946 he administered an electro-convulsive shock (ECT) first and introduced the leucotome in the post-ictal period.
There were several attempts to standardise the procedure and achieve more accuracy. Surgeons used different approaches and burr hole sites, stereotactic fixation of the leucotomes, injections of contrast to localise the lesions, and CT imaging was used.
The frequency of the procedure varied, but some estimates of the number of lobotomies between 1940 and 1969 are:
| USA | 40,000 |
| Great Britain | 17,000 |
| Sweden | 4,500 |
| Norway | 2,500 |
Indications widened, and some procedures were done on children for behaviour problems.
THE AUSTRALIAN EXPERIENCE
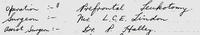
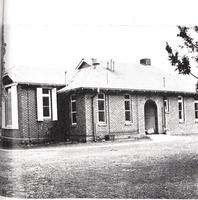
The first leucotomy in South Australia was performed by Dr. L. C. E. Lindon (later Sir Leonard) at the Parkside mental hospital in 1945. The procedure was called the "cortical undercut", indicating the incision of the frontal cortex and cutting the lower part of the frontal lobe.

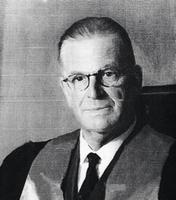
It was a favourite early procedure. As usual, aspiring surgeons at that time travelled to England to train. Two of them, T. A. R Dining and D. A. Simpson, returned as neurosurgeons and brought new techniques. They changed the procedure by using burr holes to access the frontal lobes, and used probes to avoid damage to the brain surface (the cortex). Mr Dinning performed most of the procedures.
Of the 153 such operations the results were similar to other reports. One third were improved, one third remained almost same, and one third had complications.
The Adelaide psychologists were involved in early assessments and reviewed such patients after surgery. The rule of "thirds" was the same.

Thirty Years Later
After the acceptable early results in hopeless asylum patients the indications became less rigid. Using the transorbital route, some practitioners performed the surgery in their rooms. It was inevitable that complications and criticism would follow. Haemorrhage, sepsis and epilepsy were recorded. The mortality was an unacceptable 2%, but adverse personality changes were most worrying. The noted case of Rosemary Kennedy and many others produced severe negative publicity. Freeman was likened to Dr. Mengele, a medical SS officer experimenting on inmates in Auschwitz. The Nobel Committee was urged to remove Moniz's name from from their list. Leucotomy was banned in many institutions. It is unlikely that any leucotomies were performed after 1970.
Another reason for the demise of leucotomy was the arrival of psychotrophic drugs such as chlorpromazine (Largactil) in 1951. Others followed, and the age of psycho-pharmacy arrived.
The leucotomy episode is a good example how early enthusiasm and lack of regulation can lead to unintended consequences. Some surgical disciplines can quote similar examples, mainly due to advances of medical technology.
Appendix
Psychosurgery is a branch of psychiatry which aims to treat mental disorders with neurosurgical procedures. Perhaps the best known and most infamous type of operation was the leucotomy (from the Greek "leukos", "clear" or "white", and "tomē", "cut" or "slice"), better known by its US name, a lobotomy.
Leucotomies are most effective in treating mood disorders, depression, and obsessive-compulsive disorder, but not very effective at treating schizophrenia.
During the 1930-60's, leucotomies were often done with limited external oversight, but after the discovery of drug based therapies and a growing body of evidence against them, their use was greatly diminished, if not banned. They have not been performed in SA for a long time.
Early Psychosurgery
One of the earliest forms of psychosurgery was probably trepanation, with evidence that it has been practiced since the Neolithic, ~6,500 BCE. Trepanation (from the Greek "trypanon", "borer", or "auger") involves removing a section of the skull, either by boring or by scrapping the bone away with flint, obsidian, etc. There is evidence of trepanning being used throughout most of the world, with the apparent exceptions of Australia and New Zealand. It was believed that the "evil spirits" or "demons" that caused headaches, possibly epilepsy, and other problems could be removed through the hole. The removed piece of bone was frequently kept, and may have been used as a magic charm. Another belief, and one that still exists today (despite the lack of evidence), is that by removing the bone it allows for more blood in the brain, increasing the person's level of consciousness, and making them feel happier and more energetic.
More practical uses of trepanning are to remove blood clots after injury, to allow access to the brain, to remove broken bone fragments, and to clean wounds.
The brain was not always considered to be the seat of intelligence. The ancient Egyptians believed that intelligence, emotion, and will lay in the heart ("Ib", one important part of the soul), with the brain essentially being useless stuffing. While the heart was left inside the body, and other important organs were placed inside canopic jars during mummification, the brain was disposed of.
Despite this, there is evidence (eg: the Edwin Smith Papyrus) from around the 17th century BCE) that the brain was important, noting that head injuries could cause aphasia and seizures.
This view started to change around the 6-5th centuries BCE. Alcmaeon of Croton is credited with being the first to consider that sensation and thought lived in the brain. Galen (129 AD - c. 200 or c. 216 AD) also believed that the mind lived in the brain, and also experimentally proved that specific nerves in the brain are responsible for specific muscles.
Renaissance and Modern Eras
There were few advances until the Renaissance. Andreas Vesalius (1514 - 1564 CE) dissected many cadavers, studying the brain and nervous system, and made many anatomical discoveries. He asserted that there were 7 pairs of "brain nerves" (we now know that there are 12), each with their own function.
Around 1796, Franz Joseph Gall developed his theory of "Organology", later renamed Phrenology. He proposed that the brain was made up of independent units, each with their own function, which was a revolutionary idea at the time. Gall carefully observed people and measured their skulls, and believed that he could correlate the bumps to mental and moral development and to personality traits. He divided the brain into 27 sections, which he called "fundamental faculties", and asserted that the cranial bumps were caused by pressure from these "organs", which grew with use.
Gall's theory was not well received by the Roman Catholic Church, and some scientists. The Church believed that it went against religion, while the scientists decried the lack of evidence. The Austrian government banned Gall's ideas, causing him to leave his position as a lecture in Austria, finally settling in France.
In 1808, the Institute of France formed a committee of experts to look into phrenology. They found no evidence to support Gall's theory (they were possibly "influenced" by a furious Napoleon Bonaparte, who did not agree with the interpretation of his skull).
Although phrenology had no physical proof and is considered quackery, it was useful in that it drove experimental research into the structure and function of the brain, and promoted the idea of localisation of function.
Less controversially, Gall also researched the anatomy of the brain, and improved dissection methods. Previously, dissection of the brain had been hap-hazard, but Gall worked slowly and methodically, tracing individual fibres.
Around 1825, Jean Pierre Flourens began creating localised lesions in the brains of rabbits and pigeons. By doing this, he was able to show that the main structures of the brain controlled different functions, e.g.: that the cerebrum was responsible for perception, movement, and judgement. He was unable to find specific areas for memory and cognition, likely due to the relatively simple cortices of his subjects, leading to the conclusion that they were spread across the brain. Thus Flourens was able to provide evidence for the localisation of function in the brain, and also prove that the mind was not in the heart.
Pierre Paul Broca (1824 - 1880) was able to provide further proof for this localisation. Around 1861, Broca performed an autopsy on a man who could only say "tan", but seemed otherwise unaffected mentally. Broca found a lesion, possibly caused by neurosyphilis, in the frontal lobe of the left cerebral hemisphere. He studied a further 12 aphasics, finding more supporting evidence for the localisation of speech. His work was later confirmed by several other neurologists. This area is now known as Broca's area.
Soon after Broca published his findings, Carl Wernicke began his research into the relationship between brain disease and language. He found that the damage to the left posterior superior temporal gyrus left people unable to understand words, but they could still hear normally. Wernicke believed this region (known as Wernicke's area) was connected to Broca's area.
In 1870, Gustav Fritsch and Eduard Hitzig performed a series of experiments on dogs. They electro-stimulated small regions in the exposed brain surface of conscious dogs, and noted that certain muscles contracted when specific areas of the brain were excited. This indicated a finer localisation of motor centres in the cortex. Neurosurgeon Feodor Krause did the same to anaesthetised humans undergoing tumour removal, accurately mapping the motor areas of the cortex.
This work was extended by Sir David Ferrier around 1870 - 1875. Using dogs and monkeys, he was able to find 15 different areas controlling movement. He proved that these regions controlled movement by surgically removing them, and demonstrating that the related motor functions no longer worked. He was able to predict how these regions translated to humans, providing better diagnosis and surgical guidance.
The first leucotomies on humans were performed by Gottlieb Burckhardt in 1888. He was a Swiss physician working as the Medical Director of the Préfagier Asylum in Marin, Switzerland. He believed that psychological sickness was caused by specific brain lesions. In an attempt to relieve the symptoms of 6 patients, he removed sections of cerebral cortex. He believed that this would sever communication between sensory and motor regions, with minimal damage, and could ameliorate violence and intractable conditions. Of these six, two were unchanged, two were quieter, one had epileptic convulsions, dying a few days later; and the last patient improved. He published his results, and presented them at the Berlin Medical Congress. It was not well received, and the hostile response from the medical community caused Burckhardt to stop his operations.
20th Century
The 19th century animal experiments did not show much response from the frontal lobes, leading to them being considered "silent lobes". This changed during World War I. Several cases of service men with damaged frontal lobes experiencing behavioural changes (often making puns, or telling jokes, being childish) led to the concept of Witzelsucht (from German "witzeln", "to joke", and "sucht", "yearning, addiction"). This showed that the frontal lobes had a function after all.
Leonardo Bianchi performed bi-lateral leucotomies on animals, publishing his results in 1922. He showed that both lobes needed to be removed, as one functional lobe could partially compensate for a damaged lobe.
Walter Dandy, considered one of the founding fathers of neurosurgery for his many innovations and discoveries, performed the first bi-lateral leucotomy in humans in 1930. In 1932, neurologist Richard Brickner reported that Dandy's patient seemed calmer and otherwise unaffected mentally, concluding that the frontal lobes were not the centres of intellect.
During the 1930's, John Farquhar Fulton had been experimenting on primates, comparing their location of functions to that of humans. This included performing lesioning pre-frontal cortex. He found that this produce a calming effect in his animals.
The Second International Congress of Neurology in London in 1935 featured several discoveries on the frontal lobes, including presentations by Fulton and Jacobsen, and Brickner. As part of Fulton's presentation, his junior colleague Carlyle Jacobsen brought out two chimpanzees, Becky and Lucy, who had received leucotomies. Fulton said that they had become much calmer, showing far less "frustrational behaviour". Another notable attendee at the conference was António Egas Moniz.
Moniz was a Portuguese neurologist, politician, and diplomat. He developed cerebral angiography in 1927, receiving two Nobel Prize nominations for it, and helped to develop the radio-contrast agent Thorotrast (a suspension of thorium dioxide (232ThO2), and highly carcinogenic). He is also considered one of the founding fathers of psychosurgery, controversially receiving the Nobel Prize (Physiology or Medicine) in 1949 for the "discovery of the therapeutic value of leucotomy in certain psychoses".
Moniz is believed to have thought of an operation to perform bi-lateral leucotomies in 1933, but did not implement it until 1935, about 3 months after the Neurology Congress. He believed that several mental illness were caused by fixed neural circuits, not pathology. Moniz thought that by destroying these circuits the symptoms would be cured, and that the brain would form new circuits to compensate for the damage.
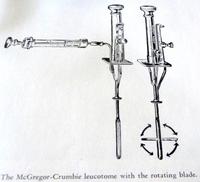
On the twelfth of December, 1935, Moniz and his neurosurgeon, Pedro Almeida Lima, performed their leucotomies at the Hospital Santa Marta in Lisbon. They trepanned into the side of the head, and injected ethanol into the "sub-cortical white matter of the pre-frontal area", destroying the connections. The patient's depression was significantly reduced, and Moniz considered the operation a success. They then repeated this procedure for the next seven patients. For their treatment on the ninth patient, they used a new device, called a leucotome ( examples of leucotomes: Wikipedia, Canadian Museum of Health ). It was an 11cm long cannula with a retractable wire loop, cutting 1cm diameter lesions.

Moniz reported his findings in March, 1936. He said that 35% (7 people) improves significantly, 35% (7) slightly improved, 30% (6) were unchanged. There were side effects, such as incontinence, apathy, and lethargy, but there were no deaths.
Leucotomy was poorly received initially, criticised for the lack of clinical observations, "degradation of personality" of the patients, and the possibility of later complications, such as meningitis and epilepsy. Despite these objections, many people began performing leucotomies in experimental trials.
Perhaps the most famous of these people was the American physician Walter Jackson Freeman II. Freeman was a strong supporter of Moniz, and introduced the leucotomy to America in September, 1936. Working with his research partner, neurosurgeon James Watts, they modified Moniz's procedure. They still trepanned into the skull, but used a blunt spatula to sever thalamo-cortical fibres rather than coring the frontal lobes with a leucotome. They named this process a "Freeman-Watts standard pre-frontal lobotomy".
Freeman though that this procedure was still too slow, and due to the need for a neurosurgeon, anaesthetist, and an operating theatre, it would be of limited benefit to those in mental hospitals. Freeman wanted a way to bring it to the public.
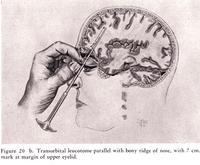
Sometime around 1945, Freeman heard of the technique developed by Amarro Fiamberti in 1937. Fiamberti punctured the patients orbital bone, and injected alcohol or formalin into the frontal lobes through a syringe, or sometimes used a leucotome instead. Freeman began to experiment with this transorbital technique, practicing on grapefruit using an icepick, and later cadavers. He first performed this operation on a live patient on the 17th of January, 1947.
Freeman bypassed the need for anaesthetics by electroshocking (using ECT machines) the patient until they passed out. He then placed an orbitoclast (jokingly referred to as an 'icepick') beneath the upper eye lid, and behind the eye. It was then tapped through the orbital bone, to a depth of 5 cm, parallel to the bony ridge of the nose, and ~15° towards the midline. The icepick was then pivoted approximately 40° away from the nose, then returned. The pick was then tapped a further 2 cm, and handle pivoted ~20° towards the nose, and then ~30° away, then moved toward the top of the head. It was then returned to the starting position, and removed. This was then repeated on the other side.
This was a fast procedure, taking about 10 minutes, as it was performed without anaesthesia, trained neurosurgeons, or a hospital stay. Watts did not approve of these changes, and the trivialising of the surgery to a simple "office" procedure, leaving in 1947.
Freeman travelled around America in his van, nicknamed the "lobotomobile", performing many lobotomies, and training staff. He was criticised for not being very selective in the patients he treated, and for trivialising the lobotomy with his theatrics. One notable case was that of Howard Dully, who was lobotomised at the age of 12, at his step-mother's request because she was fed up with his behaviour, not for any medical reason.
It is believed that Freeman performed 3,439 lobotomies, with an estimated 490 patients (~14%) dying as a result. He was eventually banned from performing surgery in 1967.
In 1947, John Farquhar Fulton proposed the destruction of the anterior cingulate cortex, a part of the limbic system, as an alternative to a standard pre-frontal lobotomy, calling it a cingulotomy. It is used mainly to treat depression, and obsessive-compulsive disorder, but was also used in Russia to treat addiction. One of the first reports of the use of cingulotomies was from the South Australian Hugh Cairns while working at Oxford in 1948.
The pre-frontal lobotomy was banned in Russia in 1950, being considered "contrary to the principles of humanity". Bans in Japan and Germany soon followed.
Another type of leucotomy was the subcaudate tractotomy, created by William Beecher Scoville around 1949. This involved boring holes in the forehead, and cutting the lower quadrants of the frontal lobes. This was later modified to use radioactive "seeds" to destroy the lobes.
The Decline of Leucotomies
With the discovery of the effective drug treatments from the 1950's, the number of leucotomies rapidly decreased. The first neuroleptic (anti-psychotic) drug was chlorpromazine, better know by the trade names Largactil and Thorazine, and first used on psychiatric patients in early 1952. This provided a much cheaper and safer treatment option, with the added bonus of not being permanent. The new drugs also significantly reduced the use of electro-convulsive therapy, insulin shock therapy, and other treatments.
The South Australian Mental Health Act of 1977 introduced a "Guardianship Board", consisting of 2 lawyers/magistrates, 2 psychiatrists, 2 psychologists, and 4 "ordinary members", chosen by the State Governor. The purpose of the Board was to protect patients, and ensure that psychosurgery was only performed as a last resort.
In 1973 and 1977, Commissions of Inquiry were conducted in New South Wales, Australia, resulting in the creation of the Psychosurgery Review Board, whose purpose was to review any psychosurgical cases. With the banning of psychosurgery in NSW in 2007, the only active review board is in Victoria. The Psychosurgery Review Board was replaced in 2014 by the Mental Health Tribunal. They received 34 applications for psychosurgery between 1988 and 2015, with no applications in 9 of those years. Applications were mostly for the treatment of extreme cases of obsessive-compulsive disorder or depression that could not be effectively treated any other way, with the application of deep brain stimulation. Its legacy will be determined by history.
Summary
From the first time they were used, leucotomies have been controversial. Their effects were unpredictable, with approximately one third of patients improving, one third mostly unchanged, and one third being negatively affected, possibly resulting in their death. It should be noted that before the discovery of effective drug therapies in the 1950's, there were few other treatments available, and they were often brutal, and mostly ineffective (eg: seclusion, straitjackets, hot/cold baths, insulin shock). In this light, leucotomies looked like a promising treatment, which ultimately failed to live up to that hope.
Since the 70's, psychosurgery has been heavily regulated, and very rarely performed. Prefrontal leucotomies are no longer performed, having been superseded by drugs, and the use of deep brain stimulation as a last resort in extreme cases.